
Written by Ronald Reed, CSPDT
Introduction
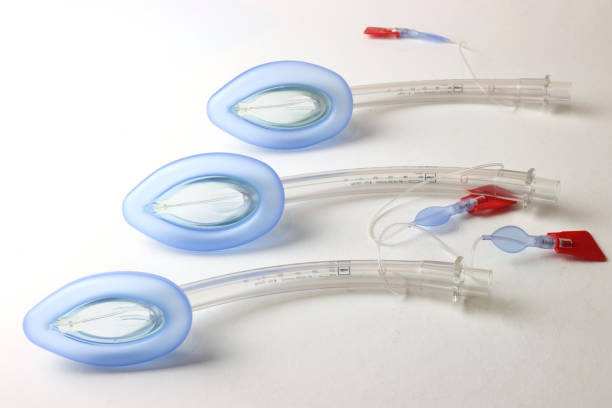
In the dynamic environment of healthcare, maintaining sterile conditions is paramount. Sterile processing departments (SPDs) play a crucial role in ensuring that medical instruments are safe for patient use. Among the many devices that require meticulous attention, the laryngeal mask airway (LMA) stands out due to its frequent use in both hospitals and surgery centers. The importance of proper LMA processing and cleaning cannot be overstated, and the differences between hospitals and surgery centers in handling these tasks highlight the need for standardized practices.
Understanding LMA and Its Importance
The laryngeal mask airway (LMA) is a device used to maintain a patient’s airway during anesthesia and in emergency situations. Its design allows for secure airway management, making it a preferred choice for many anesthesiologists. However, due to its invasive nature, the LMA must be thoroughly cleaned and sterilized after each use to prevent infections and cross-contamination.
The Processing Card: A Critical Component
A vital aspect of LMA processing is the use of a processing card, which tracks the number of times an LMA has been used and specifies when it should be discarded according to the manufacturer’s instructions. This step, though seemingly minor, has enormous consequences if not followed correctly.
Why Processing Cards Matter
- Manufacturer Guidelines: Manufacturers provide specific guidelines on how many times an LMA can be safely used. Ignoring these guidelines can compromise the device’s integrity and functionality.
- Patient Safety: Reusing an LMA beyond its recommended lifespan increases the risk of device failure, which can lead to serious complications during surgery or emergency procedures.
- Infection Control: Proper tracking ensures that LMAs are discarded before they become potential vectors for infection, thus maintaining high standards of patient safety.
Consequences of Neglecting Processing Cards
- Increased Risk of Infections: Without accurate tracking, LMAs may be reused beyond their safe limit, increasing the risk of infections like ventilator-associated pneumonia (VAP).
- Device Failure: Overuse of LMAs can lead to material degradation, increasing the likelihood of device failure during critical moments.
- Legal and Regulatory Issues: Non-compliance with manufacturer instructions can result in legal actions and penalties from regulatory bodies.
- Financial Implications: Hospitals and surgery centers may face significant financial costs due to extended patient stays, additional treatments, and potential legal fees arising from malpractice claims.
LMA Processing in Hospitals vs. Surgery Centers
Hospitals
Hospitals typically have larger, more structured SPDs with dedicated teams responsible for the cleaning, sterilization, and tracking of medical instruments. The volume of procedures and the variety of instruments processed daily necessitate stringent protocols and thorough documentation.
- Advanced Equipment: Hospitals often have access to state-of-the-art sterilization equipment and technologies.
- Specialized Staff: Larger teams with specialized training in sterile processing.
- Detailed Documentation: Comprehensive tracking systems and electronic records ensure adherence to guidelines.
Surgery Centers
Surgery centers, on the other hand, usually operate with smaller teams and may have less sophisticated equipment. Despite this, the need for meticulous LMA processing and tracking is equally critical.
- Resource Constraints: Limited access to advanced equipment may necessitate more manual tracking processes.
- Streamlined Processes: Smaller teams often lead to more streamlined but equally stringent procedures.
- Flexibility and Adaptability: Surgery centers may need to adapt quickly to changing guidelines and practices to maintain standards.
Best Practices for LMA Processing and Cleaning
- Strict Adherence to Manufacturer Guidelines: Follow the recommended number of uses and discard LMAs accordingly.
- Regular Training: Ensure all staff members are trained on the latest sterile processing techniques and the importance of accurate tracking.
- Use of Technology: Implement electronic tracking systems to monitor the usage and lifespan of LMAs.
- Quality Assurance Programs: Regular audits and inspections to ensure compliance with established protocols.
- Clear Communication: Maintain open lines of communication between surgical teams and SPDs to address any issues promptly.
Conclusion
The processing and cleaning of LMAs are critical components of sterile processing that significantly impact patient safety. Whether in a hospital or a surgery center, the use of processing cards to track the usage of LMAs is essential to prevent infections, ensure device functionality, and maintain compliance with regulatory standards. By adhering to best practices and leveraging technology, healthcare facilities can safeguard their patients and uphold the highest standards of care.
By understanding and implementing the critical steps in LMA processing, healthcare providers can ensure that their patients receive the safest and most effective care possible.
At SteriBoost, we are committed to advancing sterile processing practices through education and innovation. By becoming a member of SteriBoost, you gain access to a wealth of resources, including:
- Continuing Education Courses: Stay up-to-date with the latest techniques and standards in sterile processing.
- Expert Guidance: Learn from industry leaders and enhance your professional skills.
- Networking Opportunities: Connect with other professionals in the field to share knowledge and experiences.
- Exclusive Content: Access in-depth articles, webinars, and training materials designed to keep you at the forefront of sterile processing.
Join SteriBoost today and take the next step in ensuring the highest standards of care in your facility. Together, we can make a difference in patient safety and healthcare quality.
Visit SteriBoost.com to become a member and explore our services and benefits. Let’s work together to elevate the standards of sterile processing!
References
- Centers for Disease Control and Prevention (CDC). (2021). Guideline for Disinfection and Sterilization in Healthcare Facilities.
- Association for the Advancement of Medical Instrumentation (AAMI). (2020). Comprehensive Guide to Steam Sterilization and Sterility Assurance in Health Care Facilities.
- World Health Organization (WHO). (2016). Decontamination and Reprocessing of Medical Devices for Healthcare Facilities.
- Joint Commission. (2019). Comprehensive Accreditation Manual for Hospitals: The Official Handbook.
- Continuing Education in Healthcare
- Device Failure
- Healthcare Compliance
- Healthcare Safety
- Healthcare Standards
- Hospitals
- Infection Control
- Infection Prevention
- Laryngeal Mask Airway
- LMA Cleaning
- LMA Processing
- LMA Sterilization
- Manufacturer Guidelines
- Medical Device Decontamination
- Medical Device Maintenance
- Medical Device Sterilization
- Medical Instrument Reprocessing
- Medical Instrument Tracking
- Patient Safety
- Patient Safety in Sterile Processing
- Processing Card
- SPD
- SteriBoost
- SteriBoost Membership
- SteriBoost Services
- Sterile Processing
- Sterile Processing Audits
- Sterile Processing Best Practices
- Sterile Processing Blog
- Sterile Processing Compliance
- Sterile Processing Department
- Sterile Processing Documentation
- Sterile Processing Education
- Sterile Processing Innovations
- Sterile Processing Networking
- Sterile Processing Quality Assurance
- Sterile Processing Resources
- Sterile Processing Training
- Sterilization Equipment
- Sterilization Technology
- Surgery Centers

